|
We are thrilled to announce the addition of Dr. Michelle Guarin – please join us in welcoming her to the team!  Dr. Guarin of Natick, MA, will join the CSAH team in June. Like Dr. McCullough, Dr. Guarin treats dog, cats, and other small mammals. However, she also sees most types of birds and reptiles as well as some amphibians. We’re excited to expand our services to include the care of even more exotic species. Bring on the axolotls, bearded dragons, and ducks! Dr. Guarin grew up in Baldwin, New York. She came to Massachusetts to attend Tufts for both undergraduate and then veterinary school. She thought she wanted to be an astrophysicist but flunked calculus. She was naturally better at biology missed having pets while at school. She realized how important animals were to her and that veterinary medicine was the coolest way to mix science and animals in a meaningful way. She has been practicing veterinary medicine since 2011 in a mix of general practice and emergency hospitals, and, most recently, as the Medical Director at the Animal Rescue League of Boston. Request an appointment with Dr. Guarin or one of our other doctors! She shares her home with her husband, two young children, and a zebra finch named Niels Bohr. In her minimal free time, she loves spending time with her family at the beach and playing piano.
The addition of Dr Guarin will allow CSAH to continue accepting new pet patients while tending to our current patients. We know she will make a fantastic addition to our team. Dr. Guarin and the rest of the CSAH team look forward to continuing to serve you and your pets! Many dogs come bounding through our front doors, ready to accept our cuddles and treats and seemingly oblivious to shots and exams. But for others, a trip to the veterinarian can be a nerve-wracking experience. The unfamiliar sights, smells, and sounds can trigger stress and anxiety even in pups that are normally laid-back. With a few simple strategies, we can help alleviate their worries and make vet visits a more positive experience for our furry friends! Here are some tips to reduce stress during your dog’s next visit to the vet. What you can do even when you don’t have an appointment:
 On the day of your appointment:
Welcome to the world of pet parenthood, where every tail wag and purr is priceless! While showering your furry friend with love is essential, it's equally important to consider their health and well-being and how you can plan for their care financially. That's where pet insurance comes in – a financial safety net for unexpected vet bills and medical emergencies. In this post, we'll explore the ins and outs of pet insurance to help you in your search for the right pet insurance provider and policy. The Basics of Pet Insurance Much like human medical insurance, pet insurance is an insurance policy you can purchase that can help to lessen the overall costs of veterinary bills. If your pet is seen at by a veterinarian for a covered condition, you typically pay the bill and then submit a claim to the insurance company for reimbursement. There are three common types of plans:
Decoding the Pawlicy Before purchasing any pet insurance policy, you need to do some research so you understand to benefits and drawbacks. When we see pet owners disappointed with their insurance plans, it’s most often because they weren’t aware of what costs would not be covered. Surprises are never good when it comes to insurance, so do your research so you understand what is and isn’t covered by your plan.
A few terms you should know: Deductible: the amount you pay for covered veterinary costs before your insurance plan starts to pay. For example, if you have a $500 deductible, you pay the first $500 of covered services. Your insurer will only begin to reimburse you for covered services after you have paid your deductible. Typically the lower the deductible, the higher the cost of the plan. Premium: the amount you pay each month or year to keep your insurance policy active. Premiums vary significantly based on things like your pet’s breed & age, your policy deductible, and the cost of care where you live. Coverage limits: the maximum amount your insurer may pay out for covered claims. If you file a claim with your insurer and the costs exceed your coverage limit, then you may be responsible for any remaining expenses that aren't covered by your insurance. Some insurance policies have coverage limits for the pet for the plan year or a lifetime, some have coverage limits for each of your pet’s conditions. Exclusions: a provision in your policy that eliminates coverage for certain conditions. For example, if your pet has a pre-existing condition, such as allergies, you will not be reimbursed for any allergy-related veterinary costs. Many illness plans don’t cover the cost of the sick or emergency exam fee. These costs also won’t count toward your deductible.  Tailored Tails: What Type of Coverage is Right For You? Once you’ve explored the different types of coverage plans available, think about the plan that works for your furry friend's needs and lifestyle and for your wallet and peace of mind. While we’d love to recommend a plan that will work perfectly for your, we know that everyone’s reasons for getting pet insurance are different! A few questions you should think about when deciding on what type of plan will work best:
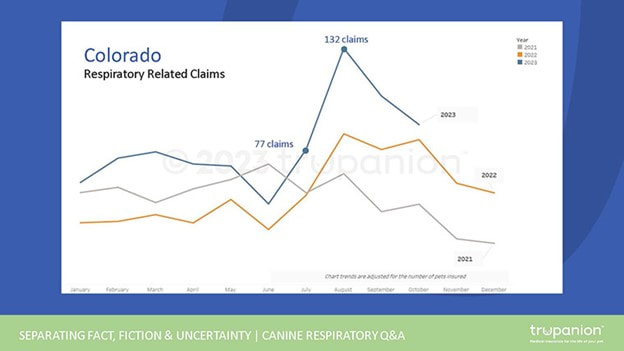
Fetching Quotes and Comparisons Now that you have a sense of the type of plan you want, it’s time to fetch some quotes from different pet insurance providers. May pet insurance providers have plan comparison tools on their website, but we typically recommend PetInsuranceReview.com as a great place to start your search. Compare plans available for your pet. Look for the right balance between coverage and cost – after all, you wouldn't want to break the bank on pet insurance treats!  What the Doctor Recommends At CSAH, we don’t recommend any particular provider or plan but we do recommend pet insurance. When your pet cuts himself in the woods and needs surgery in a specialty hospital or is diagnosed with a long-term illness that will require years of medications and care that includes regular bloodwork and vet visits, it’s a good feeling to be able to say, “yes, do it all, I have insurance.” We have one pet patient whose insurance policy has covered over $45,000 worth of veterinary expenses. Would the owner have been able and willing to pay that out-of-pocket? We can’t say, but we are 100% positive that they are glad they purchased an insurance policy! By investing in pet insurance, you’re protecting your pet but also securing peace of mind for yourself. In the worst case, you spent money on a policy you didn’t use – hopefully a policy that was within your budget. In the best, you were able to say “yes” to expensive and extensive life-saving care, care that gave your furry family member additional years of health and happiness. As usual, we’ve done our best to summarize the topic of pet insurance but we may have missed something. If you have any questions, please call us at 339-234-6007 or send us a note.  There is widespread reporting of an infectious respiratory disease among dogs that has turned deadly in rare cases. The disease has been detected in dogs across the country, including in Massachusetts. This disease is considered to be part of the canine infectious respiratory disease complex (CIRDC). What is CIRDC? CIRDC are diseases caused by several different and often highly contagious bacterial and viral pathogens and include illness such as Bordetella (kennel cough), canine parainfluenza, and canine influenza. CIRDC is endemic in dogs, meaning it’s always present wherever there are dogs. Symptoms of CIRDC include coughing, sneezing, eye or nose discharge, inappetence, and lethargy. Symptoms can last from several days to weeks. What is the canine respiratory disease observed more recently? At the moment we don’t know if this is a new disease. According to the American Veterinary Medical Association (AVMA), symptoms of this respiratory disease appear to last weeks longer than the typical symptoms of the better-known and very common Bordetella. The disease is generally resistant to standard treatments, such as antibiotics. In very rare cases, dogs develop acute pneumonia that rapidly becomes severe and often leads to poor outcomes in as little as 24-36 hours. Whether we are seeing a new disease in North America or a previously existing but undiagnosed illness is not known. In the chart below, reflecting respiratory related insurance claims submitted to pet insurer Trupanion in Colorado, we certainly see a spike in respiratory claims this fall of 2023. This increase could be the result of other factors, including a growing population of dogs, increased travel and boarding since the COVID pandemic, and delayed vaccinations and reduced socialization since the pandemic. “What the net result could be is we’ve got more dogs that have a lower level of resistance because they’ve been exposed to other dogs less over the last couple of years, and they’ve had less vaccinations. That means, just with our normal respiratory diseases that are always circulating, we’ll see more spikes in disease cases,” says Dr. Scott Weese, a pathobiology professor at the University of Guelph Ontario Veterinary College and director of the university’s Centre for Public Health and Zoonoses. Dr. Weese also states that the number of severe cases may not indicate a new disease. “When you have more cases, you’ll get more severe disease since a small percentage of dogs with CIRDC get severe disease.”  Keep your dog healthy! Whether this is a new disease or simply a bad season of CIRDC, our advice for keeping your dog safe if the same. Keep your dog up to date on vaccines. The AVMA notes that though the efficacy of existing vaccines against current cases is uncertain, maintaining your dog’s health through routine vaccinations can help support a dog’s immune system in combating disease. If your dog is a patient at CSAH, they are likely vaccinated against parainfluenza virus and canine adenovirus type 2 (part of the DHPP vaccine series given to almost all of our canine patients). At CSAH we typically only recommend Bordetella (kennel cough) if your dog is around other dogs a lot. As a pre-caution, we are recommending more dogs receive the Bordetella vaccine regardless of exposure to other dogs. If you are wondering if your dog should receive this vaccine reach out to us. We also carry a vaccine for canine influenza, but this disease is very sporadic in New England. If we hear reports of this disease in our area, we will begin recommending the vaccine. Some groomers, day cares, and boarding facilities may begin to require this vaccine as a precaution against CIRDC. Reduce your dog’s contact with large numbers of unknown dogs, such as at dog parks and using communal water bowls. Avoid nose-to-nose doggie greetings. At this point, it is not necessary to avoid day cares, boarding, or grooming facilities unless your dog or another dog in the home is immune compromised. The risk of CIRDC is not much greater than it normally is. Consider asking facilities about the vaccines they require and their cleaning protocols. If you aren’t comfortable with the answers, consider your alternatives. Keep your dog away from dogs that appear ill: those exhibiting a runny nose, runny eyes, sneezing, and coughing.  But if they do get sick Contact us immediately if your dog is experiencing a lingering cough, weakness, loss of appetite, difficulty breathing, worsening of illness, and a cough that is sufficiently severe that it causes the dog to vomit or makes it hard for the animal to breathe. Reach out early even with mild symptoms, as some cases advance very quickly. Be particularly vigilant if your dog is old, very young, brachycephalic (short nosed or flat faced), immunocompromised, pregnant, or has underlying heart or respiratory disease. While the disease doesn’t respond well to standard treatments, we can offer supportive care to help your dog fight off the infection. If your dog is suffering from a different illness, we can help identify and try to treat. Safety at CSAH Worried about bringing your pet to see us at CSAH and potentially expose them to this disease? Remember that CIRDC is endemic, so we see CIRDC cases all….the…time. We have protocols in place to prevent transmission of CIRDC and other diseases between our patients. Dogs exhibiting symptoms of diseases including CIRDC are asked to wait for their appointments in their cars instead of the lobby, exam rooms are sanitized between appointments and are disinfected with Lysol after an appointment with a patient suspected to have CIRDC or another highly contagious illness. We don’t see any more risk in bringing in your pet to CSAH than there is at any other time! As always, please reach out if you have any questions: [email protected]. Deciding when to say goodbye to a beloved companion is one of the most difficult decisions a pet owner will eventually have to face. Sometimes these decisions loom on the horizon for a while, while other times they come on suddenly and unexpectedly. No matter how long you have to plan, these choices are never easy. While you are ultimately the only person who can make this decision for your pet, we’re here to support you however we can during the process. In this article we’ll be covering some of the most common questions pet owners have when dealing with end of life planning, offering our perspectives, and linking to resources that can help you navigate these challenges, all in hopes of helping you answer the question every pet owner dreads facing: How do I know when it’s time?  Quality of Life Quality of life is a phrase you hear a lot in these conversations, but what does it actually mean? Quality of life is a broad term used to describe and average a number of factors, such as pain, mobility, hygiene, appetite, and activity. It’s important to note that quality of life is a relative term, and a “good” quality of life will look different for different pets; if you have a lapdog who’s happy cuddling on the couch, low mobility is less detrimental than it would be in a retriever who loves hiking and swimming. Some key quality of life indicators to pay attention to include:
If you're unsure of whether it's time, book a consultation with us to review your pet's health and discuss their quality of life. This is something we've all been through as well and we're here to support you.  Measuring QoL Changes in quality of life are often the first thing owners notice, and this may spark other questions or considerations. It can sometimes be hard to tell whether a pet is approaching the end of their life, or whether their symptoms are a temporary low they may recover from. Since this is a deeply emotional topic for any pet owner, it can often be helpful to use tools and outside resources to get a clearer, more objective understanding of your pet’s quality of life:
 Making Arrangements Even once you’ve decided euthanasia is the next step, you’ll likely still have plenty of questions. When should you book an appointment? What will this appointment be like? Will your pet feel pain as they pass? What happens with their remains? If you know in advance that it's time, you can call us to book your pet's final visit with us. We typically recommend that you schedule this appointment for the end of the morning or afternoon, when the hospital is a little more quiet. However, sometimes your pet declines faster than you anticipate and it becomes clear that they are in too much pain or discomfort. In this case you can call us to come in on short notice. When you arrive for the appointment a technician will bring you, your pet, and any other friends or family present into our consultation room. An intravenous catheter will be placed; this may occur in the room with you, or your pet may be brought into our treatment area while the catheter is placed, then returned to the room with you. Once the catheter is placed your pet will be administered a sedative to ease any pain and anxiety, followed by an injection that will induce loss of consciousness and death without causing pain or distress. The process is short and painless; it will be over in a matter of seconds. Your pet won’t be aware of their own passing. We partner with Final Gift Pet Memorial Center for cremation and other aftercare services, enabling them to pick up remains from and deliver ashes and memorial products to our clinic or to your home, but this is only one of the many options available to you. Some pet parents prefer to make arrangements with other pet aftercare services, or to bring their pet’s remains home for burial, both of which we’re happy to accommodate.  A Word on Grief It’s normal and expected to feel grief after the loss of a pet, just as you would after the passing of any other family member. Indeed, grief is a healthy response and an important part of the healing process. Talking about grief is one of the best ways to work through it, especially if others in your household are feeling similarly; some family members may even be thankful someone else has broached the topic. Of course, friends and family can only do so much. If you’re struggling with grief and need additional support, there are resources available. Tufts University operates a Pet Loss Support Hotline, and Ohio State University’s Honoring the Bond Program has compiled numerous readings, videos, support groups, and other resources to help pet owners dealing with grief. Grief is normal, and showing these emotions or asking for help isn’t a sign of weakness. If you’re struggling after the loss of a pet, please don’t hesitate to reach out or utilize the resources above- we know it’s what your pet would want for you.
 We’ve all heard that chocolate is bad for dogs, but there are plenty of other lesser-known pet toxins that have slapped on a costume and snuck their way into your home. To help keep your pets safe this Halloween season, here’s a list of a few of the biggest dangers to watch out for!
 So what can I feed my pet? We get it. While it’s important to keep your pet safe, you don’t want them to feel left out on a night like Halloween! If you want your dog to be able to join you in your post-Trick-or-Treat feast you can offer them a few high-value treats. You can make a game out of it with your cat or dog with an interactive food puzzle! Halloween should be a fun night, and the last place you want to spend it is an emergency room. With all that said stay safe, and Happy Halloween!  We are thrilled to announce the addition of a second veterinarian to our hospital, Dr. Stephanie Saglimbeni! Many of our clients will recognize Dr. Saglimbeni, who has been managing CSAH since it opened in the spring of 2022. Dr. Saglimbeni earned her Doctorate in Veterinary Medicine from CES University, in Medellin, Colombia. She has just completed the rigorous process that allows her to practice veterinary medicine in the United States. She is over the moon to help take care of your furry family members as a doctor at CSAH. The addition of a second veterinarian allows CSAH to continue accepting new pet patients while tending to our current patients. Dr. Saglimbeni treats dogs and cats, while Dr. McCullough treats dogs, cats, and a variety of other small animals and exotics, including rabbits and guinea pigs.
Dr. Saglimbeni shares her home with Jose, her husband, Lorenzo, her son, two cats and two dogs. In her free time, she loves going to the beach and taking pictures of wild birds.  In human medicine and veterinary medicine alike, diabetes is a scary word. If you have a pet who was recently diagnosed with diabetes, or simply like to keep yourself awake at night with a bunch of what-if worrying (no judgment, we all do it), you probably have a lot of questions about how to deal with this condition. Fortunately, it’s not all doom and gloom! While diabetes may be the boogeyman under the doggie bed, we know a lot about how to manage the disease. With proper management and a little TLC, your diabetic pet can still have plenty of happy years ahead of them. What is diabetes? Diabetes mellitus is a disease that results from the body’s inability to properly process glucose. You may have heard the words glucose and insulin in passing, but in order to understand diabetes it’s important to have a grasp of what these are, and the role they play in the body. Glucose is fuel! Specifically, it’s a kind of sugar our bodies and our pets’ bodies tend to break food into, and it serves as our primary energy source. Glucose is produced by the intestines during digestion, and is then moved to the bloodstream for transportation throughout the body. Meanwhile insulin is the hormone responsible for moving glucose out of the blood and into the other cells; glucose can travel where it pleases within your bloodstream, but it can’t actually leave without a helping hand from insulin. When these two components are working in beautiful harmony, you have a healthy happy body! But when your body doesn’t have enough insulin, or when it’s not capable of utilizing the insulin it does have, we call that diabetes. You may have also heard the phrases type 1 and type 2 thrown around. They’re not the most descriptive names, but the difference is pretty simple: type 1 diabetes means your body struggles to produce insulin, while type 2 means your body can produce insulin but can’t effectively utilize it, so glucose builds up regardless. Excessive thirst and urination are two of the most common, most recognizable symptoms of diabetes." Pet vs Human: What’s the difference? While diabetes is relatively similar across species, there are a few key differences that cause the disease to stand out in dogs and cats. For a start, diabetes tends to present later in life for dogs than it does in humans. Type 1 diabetes is usually diagnosed during childhood or adolescence in humans, while it isn’t common in dogs until middle age. Type 2 diabetes is also rare in dogs, while Type 1 diabetes is rare in cats! The other key difference sounds obvious, but it’s an important one: pets can’t take care of themselves. A diabetic human can monitor their own blood glucose, administer their own insulin, and regulate their meals as necessary, but our pets have yet to master these skills. They rely on their humans for care and may not understand why they’re being poked or denied a usual meal, which can present some extra bumps along the road. Have a diabetic pet or curious how to administer insulin? Watch our how-to video! Spotting the Symptoms The sooner diabetic treatment can be started the better, so it’s important to recognize the signs early! Excessive thirst and urination are two of the most common, most recognizable symptoms. When your blood has too much glucose the excess sugar ends up being filtered by the kidneys, which draws out additional water in the process. This water is fast-tracked to urine rather than absorbed into the body, which means our poor hypothetical diabetic dog is left thirsty no matter how much they drink. Beyond this, other major symptoms to watch out for include cloudy eyes, decreased appetite, and recurring skin or urinary infections. If you notice any of these symptoms in your own pet, give us a call and we’ll figure out next steps! Managing Your Pet’s Diabetes So you’ve got the diagnosis, and you’re wondering where to turn next. Figuring out next steps, at-home management, dietary changes, and more can be a logistical challenge and a major source of stress. Fortunately managing your pet’s diabetes actually becomes pretty simple once you get the hang of it, so we’re here to walk you through the basics! Insulin administration is probably the most recognizable part of diabetic management. If your pet can’t produce their own insulin they’ll need injections after meal time, typically twice daily, to help their body process glucose. This can be one of the most stressful parts for owners who worry about hurting their pets, but fear not! Insulin needles are very thin, and the injections are administered subcutaneously (into the layer of fat underneath the skin), so your pet will barely feel a thing. Those first few injections can be stressful, but we’re happy to demonstrate and work with you until you’re giving them like a pro. Dietary changes are another key piece, since dietary management is all about regulating those glucose levels. Veterinarians typically recommend a high fiber diet for dogs and a low carb, high protein diet for cats. If there’s one golden rule of diabetic management, consistency is key! You want to be feeding the same amounts of the same food at the same time of day, and administering the same amounts of the same insulin along with it. Ensuring that you get these routines down to a science is the most reliable way to control your pet’s insulin and glucose levels, which is the ultimate goal of treatment. Conclusion Diabetes management can be tricky. Finding the right routine can take time, and that time is often stressful for pets and humans alike. If your pet has just received a new diabetes diagnosis it may feel like too much to take in, but just remember: you’re at the hardest point right now. Every day you’ll learn a little more about taking care of your pet, and everything you learn will make it that much easier. Soon these routines will just feel like second nature! Until that time comes though, you’re not in this alone. Our staff are here to help you find a treatment plan that works for you and your pet, and to answer your questions every step of the way.  While some dogs love swimming and others won’t touch water with a ten foot stick, beaches and pools can be a summer staple for dogs of all shapes and sizes. If you plan to bring your dog around water remember that certain breeds are more suited for swimming than others (retrievers and water dogs can swim laps around boxy bulldogs), and consider the value of a doggy life-vest. If you’ve got a pool on your property, keep it covered when it’s not in use! Beaches introduce a few more unknowns, but a bit of preparation is all it takes to make your day at the beach . If you plan to let your dog off leash be sure they have a good recall, and bring plenty of fresh drinking water so they don’t try to chug the salty ocean surf. Be mindful of others as well; on a nice day there are likely to be plenty of other dogs and people, and all the new sights, sounds, and smells can make even a well-behaved dog forget their manners a bit. Enjoy that warm air, and have a great summer! In the meantime if you have any questions don't hesitate to give us a call at 339-234-6007 or email us at [email protected]  Spring is around the corner, so keep your pet safe from ticks and tick-borne illnesses! Our dogs and outdoor cats are also exposed to plenty of pesky parasites, such as ticks and the diseases they carry. The are 3 main type of ticks in Burlington, MA: Deer Ticks, an estimated 50-70% of whom carry Lyme disease causing bacteria. Dog Ticks and Lone Star Ticks. At CSAH we strongly recommend using tick preventatives such as Simparica Trio. Some clients double-up with a chewable preventative and a repellent collar like the Soresto Collar. Talk to our veterinarian to determine the best product for your pet given their health history, potential exposure to ticks and lifestyle. Use your preventative all year long! Frost and freezing temps DO NOT kill ticks. Ticks are dormant but come back to life in only 40 degrees - a high often achieved even in the coldest months. After a walk, the American Kennel Association recommends checking for ticks on your pet. Don't forget to look inside ears and between toes, just to make sure your pet didn’t bring any ticks home with them. 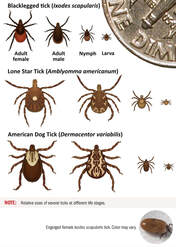 What Do I Do If I Find a Tick on My Dog? If you find a tick on your dog, remove it as soon as possible! If it hasn’t attached itself yet, there is no risk of tick-borne illness for your pet. If it has attached, grasp the tick with a pair of tweezers as close to the site of attachment as you can and pull straight back. If you have found an attached tick, particularly one that is engorged, the MSPCA advises noting the date and time to discuss with your veterinarian. Continue watching for the following symptoms*:
|
BLOG
|
|||||||||||||||
|
Contact Information:
Cambridge Street Animal Hospital 156 Cambridge St #1B Burlington,MA 01803 (339)234-6007 [email protected] Office Hours: Monday - Friday, 8am-5pm |
Join the PetPress Community!
Sign up for our monthly newsletter, the PetPress for hospital news, pet care tips and cute pet photos! |